By Tim Stephens and Keith Neely
Too often corrections administrators are incurring large, unplanned additional security costs to provide basic healthcare for lack of simple onsite capacity. Social distancing behind bars is difficult, and the number of elderly (and sicker) inmates has risen dramatically: 400% between 1993 and 2013. [1]
In early September, the U.S. Treasury issued updated guidance on “COVID-19-related expenses of maintaining state prisons and county jails.” The notice stated costs related to the “improvement of social distancing measures [and] ... compliance with COVID-19 public health precautions” were allowable. This extended the original guidance on the “building of construction of temporary structures ... and surge capacity” in Public Law 116-139, Title I (the CARES Act). [2]
COVID’s impact on corrections
Correctional facilities have been hit hard by COVID-19. Inmates and corrections officers have died from the coronavirus, and corrections outbreaks have sustained community transmission. In some states, more than 35% of the inmate population has been infected, and there are many states where the number is more than 15%.
By the middle of September, more than 125,000 people had tested positive with the number increasing by 4% per week. Infections in corrections mirror those in the general population: spiking in April, slowing in June and peaking again in August. There have been large case increases in recent weeks in Florida, California, Arkansas, Oklahoma and the federal prisons.
Corrections began to feel the impact of COVID about mid-March 2020; the first case of novel coronavirus 2019 (COVID-19) was diagnosed at Riker’s Island in New York City. According to a report from the JAMA Network, “Within 2 weeks, more than 200 cases were diagnosed within the facility, despite efforts to curb the spread.” [3] By mid-March, Cook County, Illinois faced similar conditions with about 350 incarcerated persons and staff members testing positive, and on April 19, 2020, the first inmate in the California Department of Corrections system died from COVID.
No national mandate for testing
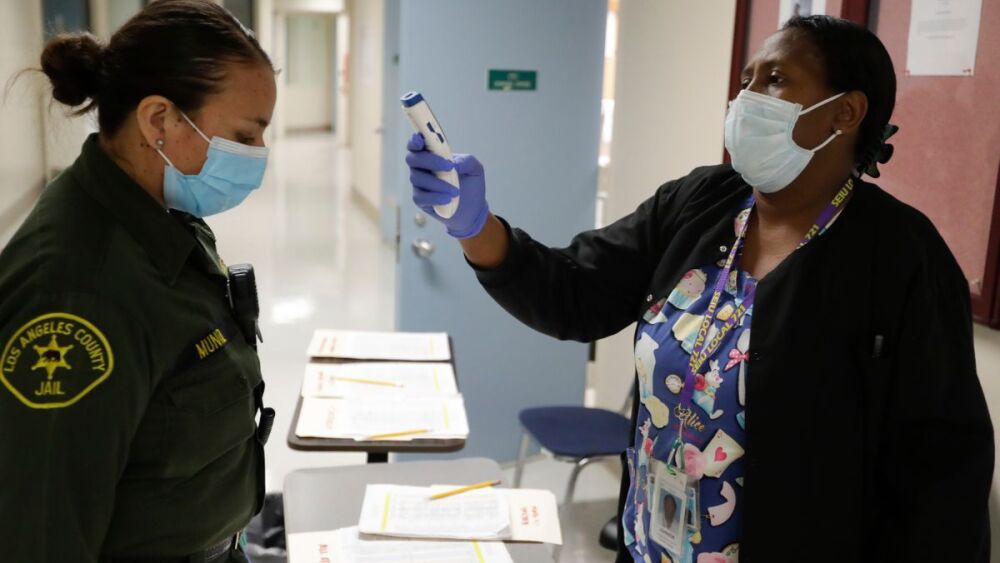
There are significant differences between the numbers of people being tested in different corrections settings, and there is no systematic or national mandate for testing corrections workers who move in and out of the jails and prisons on a daily basis. The pattern of whether the disease is moving from the community to corrections with workers, or is being spread by new inmates is hard to establish. What is clear is that the swiftness and intensity of the spread stretched available medical resources and showed gaps in the ability to isolate sick and infectious populations. Basic medical facilities and quarantine capacity can help stop the spread.
Prior viral epidemics have wrought havoc in carceral settings. An account from San Quentin prison detailing the 1918 Spanish Influenza estimated that half of the inmates contracted the disease during the first wave of the epidemic; sick calls increased from 150 to 700 daily. Contrary to protocol, most of the ill were kept in the general prison population because the hospital ward was full. San Quentin has seen more than 25 deaths during the COVID outbreak. [4]
Early release, bail waivers
Corrections officials in some states have implemented early release, bail waivers and other non-custodial programs for non-violent offenders. At present, jails and prisons are still too crowded to contain the outbreak. In Montana where the inability to transfer offenders has exacerbated outbreaks in jails where COVID-infected inmates were crowded together and further. [5] The inability to adhere to containment measures has put not just incarcerated persons, but staff and the wider community in danger.
COVID is not the only disease of concern; HIV, tuberculosis and measles all have been linked to the back and forth movement of the population between corrections and community. The movement of HIV in and out of jails and prisons in the United States has long been recognized as sustaining and extending the cycle of infection. The rate of infection among the incarcerated is more than five times that in the general population. Lack of testing, as well as lack of community treatment options for recently released inmates, compounded the outbreak from the 1990s until recently. [6]
Inmate rights to healthcare
Inmates have a constitutional right to healthcare that meets community standards. The Eighth Amendment to the United States Constitution require corrections officials to provide prisoners with “reasonably adequate” medical care. Courts have defined adequate medical care as “services at a level reasonably commensurate with modern medical science and of a quality acceptable within prudent professional standards,” and at “a level of health services reasonably designed to meet routine and emergency medical, dental and psychological or psychiatric care. [7]
Correctional administrators must adhere to best practices to avoid Eighth Amendment violations. The American Bar Association recommends that correctional authorities screen each prisoner as soon as possible upon the prisoner’s admission to a correctional facility to identify the prisoner’s immediate potential security risks, including vulnerability to physical or sexual abuse, and should closely supervise prisoners until screening and follow-up measures are conducted. [8] During this COVID era, screening can best be done in an intake setting designed for this purpose. The good news for correctional administrators is that CARES Act dollars can fully fund this.
As the COVID-19 virus continues to circulate and grow in a majority of the states, we can expect it to be a continued threat to inmates, corrections officers and the wider community as it circulates into and out of jails and prisons. We need the “all of community” effort envisaged in the CARES Act to be applied and used to help halt COVID-19 transmission in corrections.
Data cited from numerous sources including:
References
1. Maruschak LM, Berzofsky M, Unangst J. Medical problems of state and federal prisoners and jail inmates, 2011-12.
3. JAMA Network, April 20, 2020.
4. Rong-Gion Lin II, Christensen K. San Quentin’s coronavirus outbreak shows why ‘herd immunity’ could mean disaster. Los Angeles Times, August 11, 2020.
5. Efforts to Keep Virus Out of Prisons Fuel Outbreaks in Jails. U.S.News and World Report, September 26, 2020. Accessed at.
6. HIV Among Incarcerated Populations in the United States. The BodyPro, February 12, 2018.
7. Manville D. Prison Litigation News.
8. American Bar Association. General Principles, 23-2.1 Intake Screening.
About the authors
Tim Stephens, MA, is the CEO of SafeJail, a partnership of public health, facility designers, engineers and corrections experts focused on making jails safe. Tim has spent more than 30 years in developing population health innovations and public health preparedness programs. For 10 years he served as the Public Health Advisor to the National Sheriffs Association. In that role, he was the principal founder of the Emergency Services Coalition for Medical Preparedness, the combined efforts of 23 national associations to protect first responders. He served as the Director of Preparedness for the Association of State and Territorial Health Officials immediately after 9/11, and later the CEO for the largest healthcare coalition in the nation. Contact him at tstephens@safejail.com.
Keith Neely, CJM, serves as a correctional consultant for SafeJails. He is a highly experienced corrections executive with a proven ability to lead corrections professionals in the largest, fully accredited public safety agency in the United States with over 5,500 employees. Keith possesses 30-plus years of hands-on experience in correctional administration and management, security operations and investigation techniques. Keith oversaw the successful process for the Broward Sheriff’s Office, Department of Detention to maintain accreditation recognition from the American Correctional Association (ACA), Florida Corrections Accreditation Commission (FCAC), and the National Commission on Correctional Health Care (NCCHC). He served as a Commissioner for the FCAC from 2010–2016, and chaired the Nominating and Standards Review & Interpretation Committees.